In this blog Debbie Hatfield, postdoctoral fellow with Boingboing and the Centre of Resilience for Social Justice, talks about her research and what she hopes it will achieve. Debbie’s work includes promoting and developing her PhD findings which looked at patient and public engagement and involvement for commissioning health services.
How can patients, the public and health professionals work better together?

Related Resources

Can resilience be measured?
Can resilience be measured? Finding adequate and good ways of measuring is important because we would like to track the effectiveness of resilient building approaches in daily practice, to make sure that people benefit from our interventions, check the quality of our work and continue developing our interventions.
Can kinship carers benefit from learning about resilience?
This is a Collaborative Action Research project using Photo-elicitation to represent kinship carers experiences of trying to use Resilient Therapy and individual interviews with children to find out what helps them through difficult times.
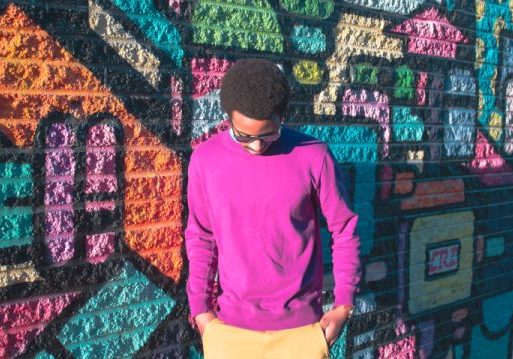
Resilience to re-offending: young men overcoming adversity
This practitioner research combines support work with young people who have experienced challenging times and the Resilience Framework. By examining the mechanisms that promoted resilience amongst young men who were offending, the study took the Resilience Framework and applied it to the data collected on the young men’s experiences.